Being overweight is a condition caused by an imbalance between calorie intake and calorie expenditure. Long-term excess body weight has many negative effects on health and increases the risk of developing chronic conditions such as type 2 diabetes, cardiovascular disease, high blood pressure, etc.
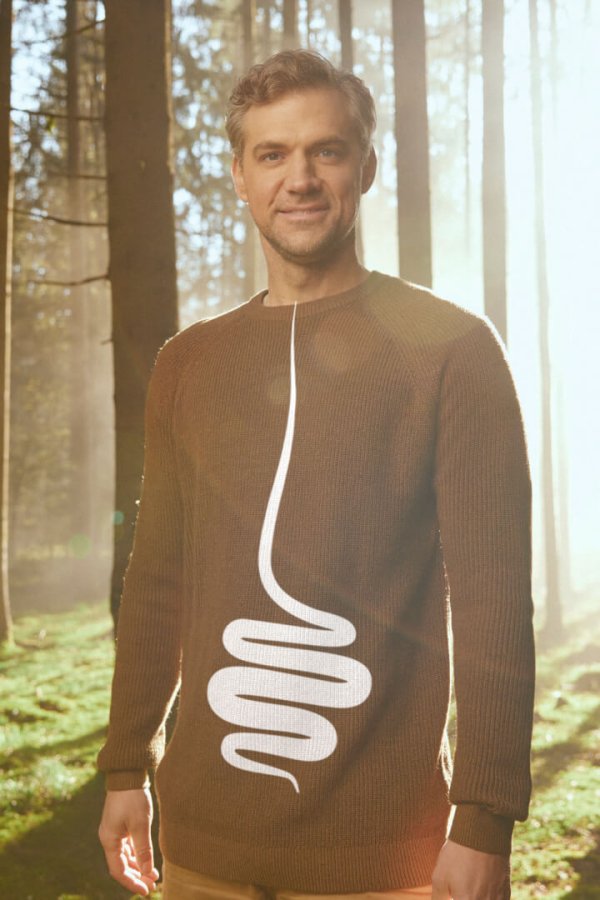
While the solution may seem simple – burn more calories than you consume – the mechanisms of obesity are extremely complex. Several mechanisms are at play before, during and after eating, which help regulate appetite, food energy intake and body weight. This article will explore how the digestive system affects body weight.
The food we eat passes through the digestive system, which is a kind of tube that stretches from the mouth all the way to the anus. The digestive system comprises the oral cavity, the oesophagus, the stomach, the small and large intestines, along with the liver, pancreas and gall bladder. Each has its own role in the digestion, metabolism and absorption of food, as well as excretion.
But it all starts in the mind, when we think about food, smell it or see it. Even in the first phase of this process, it is easy to make mistakes. Physically, digestion starts in the mouth, where we should keep food for longer than we usually do. The chewed food then travels to the stomach, from where it is gradually released into the small intestine. The speed at which the stomach empties is an important part of feeling satiated.
The gut-brain axis is the driving force behind satiety in humans. The ingestion of food causes the stomach to stretch, triggering the production of hormones in enteroendocrine cells in the intestine, which in turn stimulates a feeling of fullness and makes us want to stop eating.
And let’s not forget the “hidden organ” – the gut microbiota, which plays a key role in metabolism and can affect appetite regulation and weight gain through a number of different mechanisms and its own metabolites.
We already make mistakes in the cephalic phase of eating
The first phase of eating happens before we take our first bite of food, when we think about food or smell or see it (visual and olfactory stimulation).
This is when cephalic phase responses are triggered, which primes the body for eating. The physiological responses of the cephalic phase led to increased production and secretion of saliva, bile from the gall bladder, and digestive enzymes and hormones in the stomach and intestines, and also stimulate digestive system movement (peristalsis).

However, in our fast-paced lives the cephalic phase is often sidelined. We eat while watching TV, while working on the computer, while socialising, and we tend to order out more often than cook food ourselves.
Thus, we don’t pay much attention to food when we eat and often just cram it down our gullets. When this happens, our digestive tract is not optimally prepared to receive food and therefore functions less well. As a result, food is not fully digested and cannot be absorbed in the small intestine. Furthermore, when undigested food reaches the large intestine, it is fermented by the intestinal microbiota. This leads to flatulence, bloating, heartburn, as well as health problems resulting from nutrient deficiencies.
How do we activate the cephalic phase?
The most important thing is to remove all distractions when eating (turn off the TV, put away the computer) and eat mindfully. And what does this mean?
It means focusing on the meal in front of us, paying attention to the type of food we are eating, its smell and taste, how it makes us feel physically and mentally, asking ourselves why we’ve chosen it.
Mindful eating is the first step to achieving a healthy body weight because it allows us to improve self-control, recognise how feelings affect our eating, reduce food cravings, be aware of the amount of food we eat, and feel satiated sooner.
Read more about how mindful eating can help you improve your digestion in this article.
Do you chew your food thoroughly?
Once we put food in our mouths, we start chewing. Due to the fast pace of life and our mental disengagement from eating, we do a poor job of this task, which affects our digestive and absorption processes and the signals that regulate appetite and food intake.
There is now a large body of research demonstrating that chewing plays both a physiological and a psychological role in regulating appetite – reducing hunger and increasing satiety. Chewing for longer allows the brain to detect signals of fullness earlier. As the brain perceives satiety with a 20-minute delay, insufficient chewing can lead to overeating and an increase in body weight.

Would you say you’re a fast eater? Then pay even more attention to chewing, as this will also help you slow your eating down. To avoid being tempted to take the next bite too soon, put down your cutlery between bites.
You may have noticed that you often feel bloated after eating a meal in a hurry. One reason is that you breathe in more air when you eat quickly, and another is the amount of undigested food that reaches your large intestine, where it is fermented by intestinal bacteria and gases are produced. Fast eaters also report that they feel hungry sooner after a meal, even when they eat more than slower eaters.
In addition to regulating appetite, chewing has an important role in digesting food and ensuring access to the nutrients in what’s ingested. This is because chewing breaks food into smaller pieces, increasing the surface area accessible to digestive juices in the mouth and breaking down cell walls, thereby releasing nutrients that would not otherwise be available to our bodies.
Thus, thorough chewing facilitates and improves digestion, and ensures a more efficient absorption of nutrients. Conversely, insufficient chewing can lead to nutrient deficiencies.
Chewing is definitely the most overlooked aspect of weight management, so be sure to pay attention at your next meal and chew each bite more than 15 times. Although this may sound simple, you’ll soon realise that it takes some willpower to make effective chewing a habit.
How does the rate at which the stomach empties affect food intake?
For a long time, research did not pay much attention to the relationship between the stomach and body weight, but we now realise that, through both mechanical and hormonal processes, it plays an important role in appetite regulation and consequently food intake. Specifically, upper and lower gastrointestinal tract hormones significantly influence the appetite and the brain’s glycaemic control centres. Let’s see how.
Chewing and swallowing food activates peristalsis, the movement of digestive tract. The chewed food travels down the oesophagus to the stomach, where it is broken down mechanically and chemically. The stomach gradually stretches, resulting in a feeling of fullness.

The stomach then gradually empties its contents into the small intestine. This can take as long as 2 to 3 hours, so the speed at which the stomach empties is very important for satiety and appetite regulation.
A number of hormones released in the stomach and small intestine (CCK, GLP-1) inhibit stomach emptying to ensure optimal absorption of nutrients in the small intestine. At the same time, they act on the brain’s appetite centre, thus helping us to stop eating.
The rate of the stomach’s emptying is influenced by several factors. Some of the factors we can control include:
- the nutritional composition of the meal (e.g. fat slows down the emptying of the stomach),
- the quantity and volume of food (we can achieve a larger volume of food with little extra energy by eating vegetables),
- meal consistency (solid foods take longer to digest).
These functions of the stomach all play a role in providing short and long-term signals for controlling food intake.
The small intestine is an important endocrine organ
Most nutrient absorption takes place in the small intestine. This is where carbohydrates, proteins, fats and other nutrients are ultimately digested and enter the bloodstream.
The intestine, as the body’s digestive and largest endocrine system, serves as the central regulator of energy and glucose homeostasis. As noted above, hormones released in the small intestine regulate the rate of stomach emptying and hence appetite.
However, the composition of the gut and its function respond to food intake. Namely, intestinal cells are continuously regenerating, with a turnover of 3 to 5 days. Continuous excessive intake of food is thought to lead to poor intestinal adaptation and contribute to the development of obesity.
Studies have shown that there are differences in gut morphology and function between overweight and slim people. The length of the intestine is greater in obese people, and they also have an increased number of absorptive cells and increased intestinal permeability. Increased intestinal permeability results in increased inflammatory processes.
The large intestine is more than just an organ for defecation
Although at first glance the large intestine appears to be the final stop in digestion, studies over the past decade have shown that it has a much more important job than just removing and absorbing water. Thanks to the presence of undigested food particles, it provides a favourable environment for the gut microbiota.
The latter influences the functioning of all body systems, both directly and indirectly, through its metabolites (e.g. short-chain fatty acids), so it is no wonder that it plays a major role in our health.
The gut microbiota also contributes directly to energy intake, as it breaks down dietary fibre carbohydrates that humans otherwise cannot digest. In this way, it is thought to contribute up to 5 to 15% of the daily energy that would otherwise be unavailable to us. However, it is not fully known how much it ultimately contributes to the energy balance.

Some studies suggest that overweight people have a less diverse composition of gut microbiota, as well as a skewed ratio of fermicutes to bacteroidetes, favouring the former, which are more efficient at fermenting dietary fibre and extracting extra energy.
Eating behaviour is regulated by the gut microbiota
Given the many important functions of the gut microbiota, it is not surprising that it also plays a part in the complex process of appetite regulation, affecting the function of the brain’s reward system that drives us to seek out tasty food.
Recent studies have shown the potential role of the gut microbiota in regulating appetite through the gut-brain axis.The gut-brain axis is a bidirectional communication network that links the gut and the central nervous systems and comprises the hormonal, immune and nervous systems.
The fermentation of dietary fibre from plant food sources produces metabolites that act as signalling molecules, affecting the release of digestive hormones from the endocrine cells of the intestine, the function of the intestinal barrier, the central nervous system, intestinal nutrients sensing, modulation of the immune system, etc.
Among the most abundant microbiota metabolites are short-chain fatty acids (butyrate, acetate and propionate). While butyrate is an important fuel for intestinal cells and influences the mucosal immune system, propionate and acetate influence the release of hormones that increase satiety and suppress appetite. For example, they suppress the release of the appetite-stimulating hormone ghrelin and increase the production of the hormones PYY, GLP-1 and leptin, which in turn reduce appetite.
You can read more about gut microbiota and its impact on body weight in the following article.
However, the gut microbiota composition is highly specific from person to person, as the biggest factor influencing its diversity and composition is lifestyle, especially diet.
A diet rich in saturated fatty acids (e.g. lard, fatty parts of meat from animals) and simple carbohydrates (e.g. sweets), and low in fibre, inhibits the growth of beneficial bacteria and results in a breakdown in the ratio of good to bad bacteria.
Therefore, your diet should be predominately plant-based. A high and varied intake of vegetables and fruit, legumes, seeds, nuts and wholegrain cereals has a positive effect on the composition of the gut microbiota and the production of beneficial metabolites.
Probiotic (e.g. kefir, fermented cabbage and turnips) and prebiotic foods (onions, garlic, leeks, artichokes, asparagus, green bananas, etc.), as well as an increased intake of omega-3 fatty acids, found in oily cold-water fish and shrimp, and in seeds and nuts, will also contribute to a balanced gut microbiota.
Through the many processes that take place before, during and after eating a meal, the digestive system plays an important role in regulating body weight. The processes that occur in our bodies affect our energy intake, nutrient absorption, hormonal functions, the composition of the gut microbiota, hunger and satiety. Understanding the complex interactions between the digestive system and body weight can help us make informed dietary and lifestyle choices.
REFERENCES:
Aguirre M, Venema K. Does the Gut Microbiota Contribute to Obesity? Going beyond the Gut Feeling. Microorganisms. 2015 Apr 27;3(2):213-35. doi: 10.3390/microorganisms3020213. PMID: 27682087; PMCID: PMC5023237.
Feinle-Bisset C, Horowitz M. Appetite and Satiety Control-Contribution of Gut Mechanisms. Nutrients. 2021 Oct 17;13(10):3635. doi: 10.3390/nu13103635. PMID: 34684635; PMCID: PMC8539844.
Goh AT, Choy JYM, Chua XH, Ponnalagu S, Khoo CM, Whitton C, van Dam RM, Forde CG. Increased oral processing and a slower eating rate increase glycaemic, insulin and satiety responses to a mixed meal tolerance test. Eur J Nutr. 2021 Aug;60(5):2719-2733. doi: 10.1007/s00394-020-02466-z. Epub 2021 Jan 2. PMID: 33389082.
Goyal RK, Guo Y, Mashimo H. Advances in the physiology of gastric emptying. Neurogastroenterol Motil. 2019 Apr;31(4):e13546. doi: 10.1111/nmo.13546. Epub 2019 Feb 10. PMID: 30740834; PMCID: PMC6850045.
Krop EM, Hetherington MM, Nekitsing C, Miquel S, Postelnicu L, Sarkar A. Influence of oral processing on appetite and food intake – A systematic review and meta-analysis. Appetite. 2018 Jun 1;125:253-269. doi: 10.1016/j.appet.2018.01.018. Epub 2018 Feb 22. PMID: 29408331.
Lasschuijt MP, Mars M, de Graaf C, Smeets PAM. Endocrine Cephalic Phase Responses to Food Cues: A Systematic Review. Adv Nutr. 2020 Sep 1;11(5):1364-1383. doi: 10.1093/advances/nmaa059. PMID: 32516803; PMCID: PMC7490153.
Lean, M., Malkova, D. Altered gut and adipose tissue hormones in overweight and obese individuals: cause or consequence?. Int J Obes 40, 622–632 (2016). https://doi.org/10.1038/ijo.2015.220
Miquel-Kergoat S, Azais-Braesco V, Burton-Freeman B, Hetherington MM. Effects of chewing on appetite, food intake and gut hormones: A systematic review and meta-analysis. Physiol Behav. 2015 Nov 1;151:88-96. doi: 10.1016/j.physbeh.2015.07.017. Epub 2015 Jul 15. PMID: 26188140.
Zanchi D, Depoorter A, Egloff L, Haller S, Mählmann L, Lang UE, Drewe J, Beglinger C, Schmidt A, Borgwardt S. The impact of gut hormones on the neural circuit of appetite and satiety: A systematic review. Neurosci Biobehav Rev. 2017 Sep;80:457-475. doi: 10.1016/j.neubiorev.2017.06.013. Epub 2017 Jun 29. PMID: 28669754.
Choose chapter: